About us

Who we are
The Obesity Collective is the peak body for obesity in Australia. It is a national umbrella coalition with a vision to reduce the health and wellbeing impacts of obesity in Australia. Working together to raise awareness of the science and reality of obesity and promote evidence-based prevention and treatment action through a strong, cooperative and inclusive network.
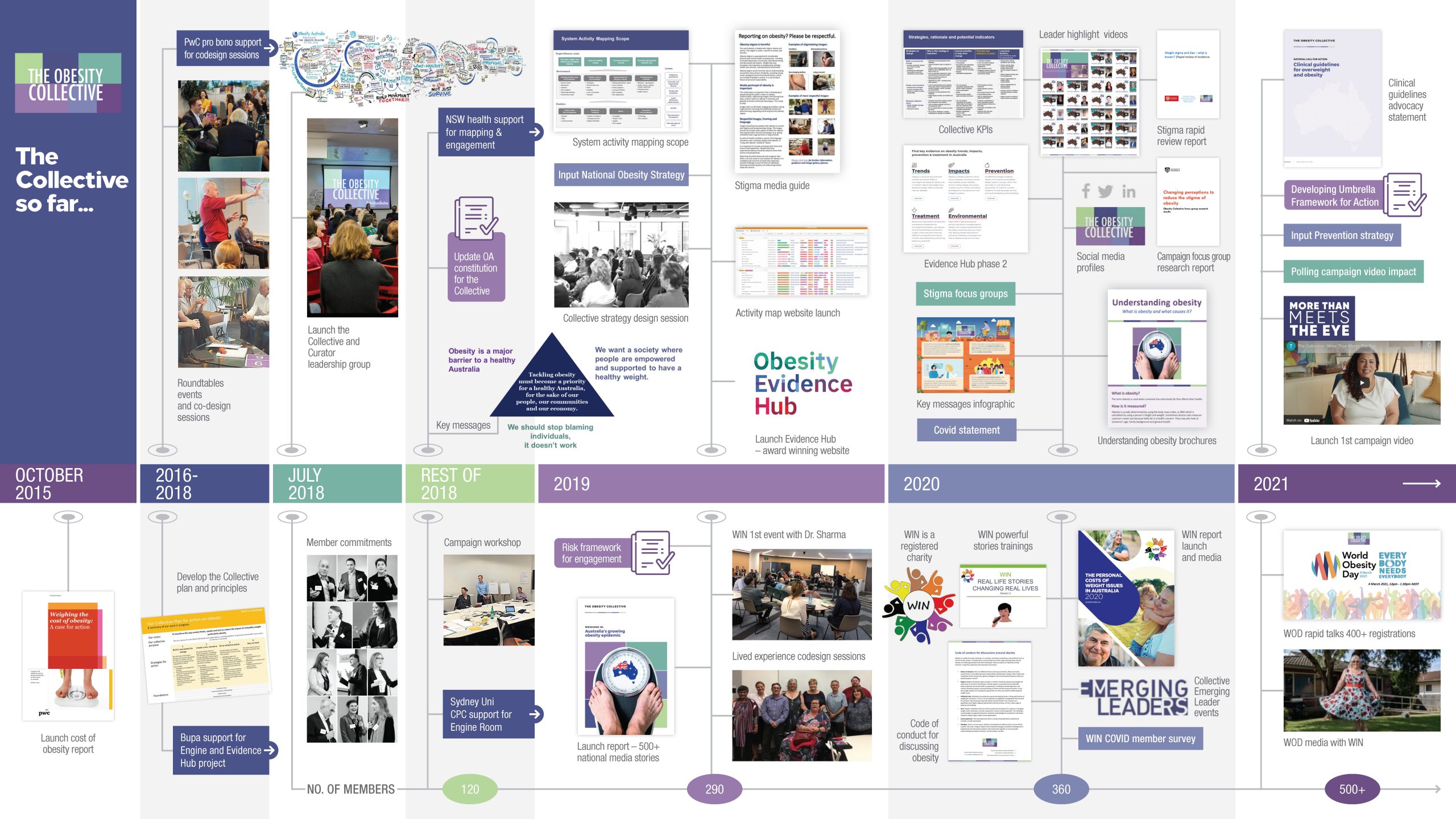
The Obesity Collective was launched in 2018 in response to the growing recognition that obesity is a systems challenge that is misunderstood and that we need to do more about it for the health and wellbeing of Australians.
The Collective evolved through codesign with a broad range of obesity prevention and treatment experts as well as social change and community leaders. We came together to brainstorm how we can look at obesity differently for the benefit of the community and to overcome some of the usual and major barriers to action including:
- The oversimplified and stigmatising view the obesity is just a personal choice
- A false dichotomy that either prevention or treatment require attention and investment when both are needed
- There are no ‘silver bullets’ for obesity and complex systems change is need which requires collaboration across many areas
The Obesity Collective is supported by two leadership groups, the Obesity Australia Board and the Advisers group. We have a national membership with members from hundreds of Australian organisations.
Together, we are transforming our understanding of obesity and how to address related challenges.
We are collaborative; we encourage knowledge-sharing, cooperation and innovation to advance evidence informed projects, programs and services related to obesity.
The Collective focuses on systems level projects which evolve each year. Some examples include:
- Sharing the latest evidence and research through communications and the Obesity Evidence Hub.
- Advocating for the National Obesity Strategy and updating the National Clinical Guidelines.
- Identifying activities and action opportunities through system activity mapping.
- Collaborating with the Weight Issues Network to address weight stigma and share the lived experience perspective.
- Developing thought leadership reports and presentations to help raise awareness of the science and reality of obesity.
- Support research initiatives that help address important gaps in the system.
- Campaigns to reducing stigma in the healthcare system and society more broadly.
Vision:
An Australia where healthy communities prioritise health and wellbeing, and where weight and obesity are treated as collective responsibilities – free from stigma and shame.
Mission:
We work towards a whole-of-society response to obesity and addressing weight stigma through collaboration, knowledge-sharing and research. Our purpose is to transform the way society thinks, speaks and acts on obesity.
Obesity Collective guiding principles
We need to step up. As individuals, as a collective, as a society.
The Obesity Collective’s work is guided by these core principles.
1.
We work to fight weight stigma
We recognise that stigma is based on misunderstanding the science and reality of obesity. It is harmful and holds us back from valuable action.
2.
See the whole picture of obesity
Obesity exists on a complex, interconnected continuum of prevention and treatment. We reflect this in our advocacy and avoid single-issue interventions.
3.
Strive for a whole-of-society approach
We are taking a systemic approach that considers the social, biological, political, economic and cultural drivers of health and health inequalities.
4.
We’re stronger together
Every organisation in the Obesity Collective is committed to leaving their agendas at the door and prioritising collaborating on equal footing.
5.
Be flexible and growth-oriented
We will continue to adapt our strategy and plan as we go, based on what we learn in practice.
Our people
The Obesity Collective has over 900 members from across the country and in each state and territory.
We have members from hundreds of diverse organisations, with examples including professional medical colleges, community and consumer groups, indigenous organisations, the Australian and State Health Departments, large corporates, other charities and peak body organisations, social enterprise start-ups, academic institutions with top national and international experts, preventive health and clinical experts, other social services as well as committed individuals and lived experience representatives.
Our goals and how we’ll get there
The condition of obesity can have serious impacts on people’s health and quality of life. The challenge is complex, with multiple, overlapping factors operating at many levels, from individual biology to the whole of society. Solutions must reflect this complexity as well. We need to tackle the challenge collectively with a system and whole of society approach.
To reduce the impact of obesity on people’s health and wellbeing, systems level thinking and a broad range of interventions are required such as policy changes, healthier environments, reducing stigma, targeting social, economic and commercial determinants of obesity, and access to quality care for those who experience the health impacts of obesity.
Build a movement, community and shared understanding
The Obesity Collective champions a whole-of-society approach to obesity. This means building a movement for change that works across all parts of society.
We are working to convene and connect members and those interested across the system. Through leading research, cross-sector events and knowledge-sharing, the Obesity Collective increases community demand for and participation in a whole-of-society response to obesity.
Create a new narrative and Improve understanding of the challenge
Weight stigma and bias means the word obesity is loaded with blame and shame. Weight stigma is unfair, harmful and a key barrier to action. Behind weight stigma is a misunderstanding of the drivers of obesity and the perception that it is a failure of personal responsibility.
We are working to change the narrative around obesity to reduce stigma, increase understanding of the science and shift focus to action beyond blaming the individual.
The Obesity Collective is committed to elevating the voices of those living with overweight or obesity and collaborate with the Weight Issues Network to do so. Connecting those with lived experiences with key decision makers and sharing their stories is key to a successful whole-of-society response to obesity.
Generate collective action and policy change
The Obesity Collective is committed to a systems and social movement response to obesity. Through cross-sector collaboration, research and knowledge-sharing, the Obesity Collective helps identify strengths and gaps in society. From here we can mobilise our members and expertise to support collective action, systems change and shape future policy decisions.
Collective leadership
Obesity Australia Board
Obesity Australia is the legal entity and oversight body for The Obesity Collective. Obesity Australia is served by a Board who have demonstrated leadership in their field such as public affairs, politics, health and public policy.

Prof Stephen Simpson AC FAA FRS

A/Prof Annette Schmiede

Prof Emeritus Ian Caterson AM FRSN

Ms Sue Bellino

Mr Andrew Wilson

Prof Caroline Miller

Mr Alan Garner
Obesity Collective Advisers
The Obesity Collective has over forty Advisers across Australia. The group represents a diverse range of perspectives and expertise in preventive health, clinical healthcare, systems change, policy, lived experience and population health. The group come together regularly to share strategic insights, discuss current opportunities and action areas as well as provide input for statements and resources.

Prof John Dixon

Prof Steve Allender

Dr Jo Mitchell

Dr Georgia Rigas

Adj Prof Louise Sylvan

Dr. Alex Craven

A/Prof Samantha Hocking

Dr Shirley Alexander

Jenna Van Der Velden

Dr Jaithri Ananthapavan

Prof Brian Oldfield

Ms Elizabeth Calleja

Ms Catherine Smith
Dr Dorota Sacha-Krol

Prof Leonie Heilbronn

Prof Helen Skouteris

Dr Catherine Bacus

Ms Carrie-Anne Lewis

Dr Kathryn Williams

Prof Anna Peeters AM

Prof Rosemary Calder

Dr Daisy Coyle

Mr Benyamin Hakak-Zargar

Dr Hiba Jebeile

A/Prof Gary Sacks

Ms Stephanie Heard

Ms Kristie Cocotis

Dr Terri-Lynne South

Dr Anna Wood

Prof Louise Baur AM Pres FAHMS

Ms Deanne Minniecon

Prof Stephen Colagiuri OA

Jane Martin BA MPH Hon Doc

Laureate Prof Clare Collins OA, FAHMS

Ms Clare Mullen

A/Prof Priya Sumithran MBBS (Hons), PhD, FRACP

Mr David Burns

Prof Amanda Lee

Prof Nuala Byrne

Dr Kimberley Norman

Dr Blake Lawrence

Prof Stephen Simpson AC FAA FRS

Ms Judy Nean

Nadia Mastersson

Prof Kathryn Backholer

Dr Teresa Girolamo

Anthony Okely
Stigma Expert Group
A team of stigma researchers and experts from different organisations who work together to understand the current evidence and different perspectives of weight bias, stigma and discriminations. Their work helps inform the stigma work of the Obesity Collective.

Dr Elizabeth Holmes-Truscott

Dr Briony Hill
Dr James Kite

Dr Zanab Malik

Prof John Dixon

Dr Blake Lawrence

Dr Joanne Rathbone

Dr Timothy Broady

Dr Xochitl delaPiedadGarcia

Dr Kimberley Norman
Obesity Collective Core Team
We have a small but mighty team of two paid staff at the Obesity Collective that is responsible for the daily management and coordination of the organisation. Collectively, this team brings strategy, business management, project management, engagement and administration.

Monica Garner

Prof Tim Gill
Collective members
The Obesity Collective has a broad membership base across the country. We have members from hundreds of diverse organisations, with examples including professional medical colleges, community and consumer groups, indigenous organisations, the Australian and State Health Departments, large corporates, other charities and peak body organisations, social enterprise start-ups, academic institutions with top national and international experts, preventive health and clinical experts, other social services as well as committed individuals and lived experience representatives.
Members decide the level of engagement and contribution that works best for them based on their time and resources. Some members are very actively involved in our work and volunteer on a regular basis, while others participate and share our messages when they can.
Who can become a member of the Obesity Collective?
The short answer is anyone who shares our values is eligible. We bring together those who are passionate about challenging the current personal blame narrative on obesity and advocating for society-wide action.
It doesn’t cost anything to become a member. However, it is important to us that our members are aligned with our vision and principles:
- Obesity is an important societal topic that requires action – to create healthier environments for everyone and better support for people who want to manage their health.
- Blaming individuals for obesity doesn’t work, and is harmful.
- We need systems change, and responsibility needs to be shared throughout all sectors for a healthier Australia.
- We need to collaborate and work in new and different ways to achieve collective impact.
- We are inclusive, anti-stigma, mindful of health inequalities, informed by the evidence, and focused on the whole picture.
Contributions to the movement include time, expertise, research, funding, networks, obesity programs and initiatives or information.
General FAQs
What is the Obesity Collective?
The Obesity Collective is the peak body for obesity in Australia. It is a national umbrella coalition with a vision to reduce the health and wellbeing impacts of obesity in Australia. Working together to raise awareness of the science and reality of obesity and promote evidence-based prevention and treatment action through a strong, cooperative and inclusive network.
Who does the Obesity Collective represent?
Obesity is a ‘systems challenge’ which requires a broad range of actions across society to create healthier environments and better support people with obesity to achieve their health goals with evidence-based treatment and care options. No one program or initiative will solve obesity.
Our members represent the many different areas relevant to obesity including public health, research, clinicians, education, community and consumer groups, businesses and innovators, other peak bodies with aligned interests, people with lived experience of obesity and state health departments.
Why was the Obesity Collective established?
The Obesity Collective was launched in 2018 in response to the growing recognition that obesity is a systems challenge that is misunderstood and we need to do more about it for the health and wellbeing of Australians.
People with obesity are not treated fairly in society, including by the health system, due largely to a lack of understanding or a misunderstanding of the science and reality of obesity. The rise in obesity prevalence in the last few decades is largely a biological response to an ‘obesogenic environment’ that promotes weight gain. It is critical that people in general and particularly healthcare professionals understand that obesity is more than just a failure of personal responsibility. There are also strong social, genetic, biological, historical and environmental influences outside of people’s control. For some communities, such as Aboriginal and Torres Strait Islander peoples, the historical contexts are relevant. For example, the impact of trauma and removing people off their land affects their health, wellbeing and the way they eat for generations and into today.
To take on systems change and to change the narrative around obesity, you need a broad range of community leaders and a collective approach.
What does the Obesity Collective do?
- Create a membership network and community of a shared understanding and collaboration. Share progress, action opportunities and new research insights. Work together to change the narrative and focus on evidence-based change needed. More on membership here.
- Change the narrative around obesity. Working to increase understanding of the science, reduce harmful weight stigma, and shift focus to action beyond blaming the individual through communications, resources, media, presentations and supporting the voice of those with experience of obesity. Check out our resources here.
- Communicate the need for action, beyond blaming individuals. We support action on evidence informed prevention and treatment initiatives, help identify and advocate for systems action such as the need for healthier environments for everyone, a National Obesity Strategy and new clinical guidelines in Australia. See our statements to find out more.
What is the relationship between the Obesity Collective and Obesity Australia?
Obesity Australia is the legal entity and oversight body for the Obesity Collective. Obesity Australia was established in 2012 under different leadership and has evolved, including a constitution update, to support the goals of the Obesity Collective which launched in 2018.
Who funds the Obesity Collective?
As the operating arm of Obesity Australia, the Obesity Collective accepts donations from a range of donors. Obesity Australia is a registered charity and receives funding from federal and state government and non-government sources. Our major funders since 2018 have been NSW Health, BUPA Health Foundation, the Australian Commonwealth, and the University of Sydney.
We have also received smaller project-based grants from Novo Nordisk, Amgen and Johnson and Johnson with the last grants received in 2019 and 2020.
Why have we taken a collective approach to the challenge of obesity?
Most people don’t understand obesity and assume it is as simple as just a personal choice which is inaccurate, and this oversimplification drives harmful stigma. Obesity is complex with social, biological, political, economic, and cultural drivers. This means that a whole of society approach is needed to change the narrative and drive action. This requires representation and united voice across a range of perspectives and expertise areas include prevention, treatment and lived experience.
What are the benefits of being a member of the Obesity Collective?
People and organisations typically join the Obesity Collective because of their firm conviction that we need greater action and a systems-based approach to obesity in Australia. Through our network, our members can connect with each other and share information; keeping up to date on information, opportunities, and activities in the obesity space.
What is the Obesity Collectives relationship to other obesity-related organisations?
As the peak body for obesity in Australia and an umbrella organisations, we work collaboratively with many other organisations who focus on obesity including the Australian and New Zealand Obesity Society (ANZOS), Weight Issues Network (WIN), Australian and New Zealand Metabolic and Obesity Surgery Society (ANZMOSS), Obesity Policy Coalition (OPC) and National Association of Clinical Obesity Society (NACOS). We are a member of the World Obesity Federation.
The Obesity Collective is supportive of WIN in providing a voice of lived experience of obesity. We work to help ensure that WIN is included in discussions about weight stigma, obesity treatment and care. WIN directors sit on the board of the Obesity Australia and the Obesity Collective leadership team, to help set and guide the strategy for the Collective.
‘Obesity’ is a loaded word. Why does the Obesity Collective use it?
Some feel that the word obesity should not be used because of the shame and blame associated with it. Our position is that obesity is a medical term that can be used respectfully. It is a description of a condition, not a label or personal judgement. As we have seen with other stigmatised health challenges in the past (e.g., cancer, depression, and diabetes), avoiding a word is confusing and not necessarily helpful in reducing stereotypes. Talking around the topic or using other words to describe high levels of adiposity that impact health will only create new words that are loaded with stigma and blame. We are working to raise awareness and reduce stigma around obesity, primarily as a condition, but also as a word.
Can the Obesity Collective help me with health advice or to find obesity services?
The Obesity Collective is principally a small policy, education and advocacy charity organisation. We are not qualified or resourced to provide medical advice to individuals. We recommend that you make an appointment with your GP or other trusted healthcare professional to discuss options.